A change in appetite is a normal part of the aging process, but it is essential that you monitor mom and dad to ensure they maintain proper nutrition. Although many seniors tend to eat less as their metabolism slows and their nutritional needs change, there are some factors that could signal a more serious problem.
So When Should You Be Concerned?
A lower metabolic rate and lessened physical activity results in a general need for fewer calories, which is normal as we age. It is also normal to have appetite changes related to dental problems, gastrointestinal changes (like lactose intolerance) along with changes of smell and taste which can affect your loved one’s enjoyment of food. However, if your parents are choosing foods that are primarily non-nutritious or they are only eating a few bites at meals or skipping meals all together, then it’s time to take a more serious look at why. To rule out any underlying health problems, it is always a good idea to consult a physician.
What Are Some of the Possible Reasons for Appetite Loss?
While some of the factors associated with a loss of appetite in the elderly can be considered minor in their severity, others are more serious and definitely require a bigger cause for concern and immediate attention. Any unexplained changes to your loved one’s dietary health, including unexpected weight loss, weight gain, or general malaise, should be checked out by a physician as soon as possible. Let’s start by examining some of more common reasons:
1. No longer feels like cooking
Standing on their feet in front of a hot stove or oven can become exhausting as we get older. With seniors’ generalized weakness and decrease in physical activity, even a “quick” 15-20 min meal preparation can lead your parent feeling tired with leg aches and pains and needing to sit down and take a rest. As a result, many caregivers opt to cook for their parents, or use meal delivery options such as Meals on Wheels, Silver Cuisine or Healthy Chef. If your parent is still able to use the microwave safely, then soups, sandwiches, cereal, oatmeal and frozen meals are easy options. Just be sure that you monitor their choices to ensure they are getting quality nutrition, as many of those “convenience” foods are largely unhealthy. You may also want to consider an in-home care professional who can assist with going grocery shopping, making light meals, ensuring proper nutritional intake and cleaning up around the house.
2. Changes in senses for taste, smell and vision
Eating involves multiple senses and because our sense of smell is very closely tied to our ability to taste, changes in any of our senses can directly influence our appetites. A dulling of taste, smell or even our vision can leave us feeling less hungry or eager to eat. To help enhance the dining experience, alter recipes to include more flavorful spices, herbs and vegetables. Use aromatic techniques to create more flavorful profiles and help trigger mouthwatering aromas in the process.

Although you might be tempted to add increased sugar, salt, and fat to a senior’s diet – Don’t! Although it is is an easy method of intensifying the flavors of their food, it is unhealthy. Instead, opt for fresh herbs, a squeeze of citrus, spices, extracts, and different cooking techniques to boost flavor and aroma profiles. Also note that many seniors, particularly those with dementia tend to favor mostly sweets. If your loved one seems to be eating a lot of desserts, then try to modify their meals to include sweeter foods and be sure they get enough of all the food groups. Some ideas for use of healthy “sweets” is to substitute sweet potatoes for mashed potatoes, use fruits as snacks, add fruit and scoop of flavored protein powder to oatmeal or use honey as a natural sweeter on vegetables. And to make the meal as more visually appealing, use a plate that contrasts with the food being served and choose healthy, bright-colored foods that are separated on the plate to allow for your loved one to discern what they are eating. Try to vary the plate presentation daily so they don’t become “bored” with meals.
3. Medication side effects
Some of the commonly prescribed medications for seniors can have an impact on their appetites, particularly those related to anti-depressants, stimulants, and dementia drugs. Ask your physician or pharmacists to determine if one of their medications may be the culprit in their reduction of appetite or could be causing directly related symptoms such as constipation, nausea, diarrhea, vomiting or dry mouth. If the problem is dry mouth, then chewing sugarless gum, brushing often or using an oral rinse prior to meals can improve taste sensation, and ultimately nutrient intake. If water doesn’t taste right, try adding herbs, or sliced fruits or veggies like lemon or cucumber.
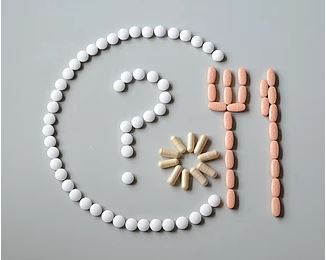
Another side effect of certain medications causes changes in taste buds that makes food tastes “bad”, often described as metallic tasting food or drinks. If the meat is tasting “off”, then try other sources of protein like diary or beans. Food substitutions can be made for most any food group. Consult their physician as they may be able to adjust their medications regimen in order to minimize these negative side effects.
4. Constipation
Perhaps they have had stomach issues for all their lives or perhaps they are on a medication (particularly those for pain) which is causing your loved one to have increased gastrointestinal issues. Slower digestion is common during the aging process ad can become very uncomfortable. Symptoms of constipation include a feeling of fullness which can prevent seniors from eating properly. As a general rule, it your parents have gone more than 3 days without having a bowel movement, or they have struggles when the do go tot the bathroom, then try to increase their fiber and fluid intake and encourage them to engage in some form of physical exercise as often as possible. This can include a neighborhood walker 10-15 min, dancing in the living room or just some simple stretching or yoga poses may help get things moving.

Try to avoid using laxatives, which are not intended for long-term use and can actually make the situation worse. If the problem persists, speak with a physician about additional steps to take.
5. Depression or Loneliness
It has long been a pastime that social gatherings are centered around food and drink. Many of the seniors today come from families where the whole family sat down together for dinner at the dinner table to discuss their day. Therefore they associate meals as being shared with other people, so if your parent is single or widowed, the lack of social interaction could be the cause of their reduced appetite. If possible try to set up social dates where mom or dad is able to go out and meet some friends for lunch at a restaurant, or have someone come over to the house to share a lunch or dinner together.

Recruit family, friends and neighbors to join them regularly for meals, or even just an after noon snack. Sitting down with mom or dad even once a day to just simply converse and share a bite can have tremendous benefits for those who crave the social aspect of eating. If you have time, attend “food dates” like those gatherings hosted at community fairs, senior centers or church functions or check your local Area Agency on Aging to find planned events and resources to encourage socializing and their appetites. Studies show that people eat more when they are with others.
6. Oral health or swallowing problems
Oral care is extremely important as we age as there are many risks associated with poor oral hygiene. The shape of the mouth and jaw can change steadily over time that can result in increased difficulty chewing or developing ill fitting dentures which can cause painful sores and irritation in the mouth. Regular dental checkups can prevent serious problems from occurring and help seniors continue to eat normal foods.
In some cases, seniors become deconditioned and struggle with the energy to eat entire meals that require extensive amounts of chewing.

You can break up the meals and try having them eat 5 small meals per day, instead of 3 bigger ones. It may be also be necessary to serve foods that are soft, moist and cut into smaller pieces in order to make it easier for mom or dad to consume, particularly if they are experiencing oral discomfort or swallowing difficulties. For example, serve vegetables cooked instead of raw. Avoid steak and pork chop, and opt for fish, or recipes that include ground meat, or cuts that can be cooked until tender. Also serving meals with healthy sauces can moisten ingredients and facilitate chewing and swallowing as well. Some of the common signs that your loved one may be experiencing swallow problems include coughing, throat clearing or sneezing at meal time, drooling or regurgitation, having pain during swallowing or feeling lump in throat. If any of these symptoms are present in your parent, you should seek the help of a speech-language pathologist immediately as severe swallowing problems can lead to pneumonia and even death. If you are worried that your loved one is not getting enough protein as result of a swallowing problem, then use milkshakes with protein powder to supplement their diets and serve it to them throughout the day or leave it for them in a pitcher in the fridge so they can have it anytime. The sweet taste of these shakes can make it a preferred drink, particularly if they are not a big fan of water.
7. Loss of appetite due to health conditions
Changes to taste or appetite can occur in conjunction with some serious illnesses, including head and neck cancers, thyroid disorder, mouth and throat infections, Parkinson’s and Alzheimers. In addition, if a senior is suffering from depression they may a condition call Adult Failure to Thrive, or AFTT, or anorexia in adults . Chronic health conditions, such as diabetes, can damage digestive-system nerves and slow stomach emptying in addition to developing constipation which can make your parent feel full after only a few bites.

Dementia can make people feel indifferent about eating (amongst other things), and the progressive brain damage it causes may mean your loved one can no longer sequence the steps and needs to be fed by a caregiver. A stroke or advanced Alzheimer’s can lead to swallowing problems and chronic obstructive pulmonary disease (COPD) can make breathing difficult while eating requiring additional energy and time. As we age, there are multiple reasons that our appetites change, as we as caregivers must be diligent in monitoring exactly what is happening with our loved one in order to keep them functioning at their best. Without proper nutrition, there will be no energy for the body to fight off infections or manage their day-to-day needs.
What Are Some General Strategies to Improve Intake?
Although we have shared some of the most common reasons for appetite change and some suggestions for remedying the situation, here are a few more things to consider trying. If you loved on has a general lack of appetite and you fear they are not getting adequate nutrition try providing nutrient-dense foods versus trying to increase the amount of food they eat. Adding extra healthy calories from food like olive oil, avocados or even a little peanut butter can help with packing in the calories. If you try to serve them large portions at meals, it may backfire and they become overwhelmed by the amount of food on the plate and end of eating only a few bites, if anything. If this happens, try separating each food into a separate bowl and presenting the bowls one at a time. This is a particularly useful strategy for those with dementia who struggle with remembering that they may have already eaten, but can be visually inundated with the amount of food they are expected to eat, particularly if they struggle with intake as it is.
It may also help to set a regular eating schedule. As humans, we tend to be patterned and routine. Our bodies tend to thrive off regularity, as do our hunger and thirst signals, so when we deviate from our normal routines, so does our appetite. If your loved one has gotten off course, serve food at roughly the same time every day. It is not a good idea to rely on your parent to tell you when they are getting hungry as that severely decreases as we age. If they are not eating regularly, start off slowly by adding a small beverage and/or snack during their normal meal time. This can help adjust their internal clocks and get the body’s hunger signals going again. You may also want to try serving a liquid meal supplement as a snack between meals to improve their healthy caloric intake. These shakes not only provide extra calories, but also contain carbohydrates for energy, supplemental vitamins and minerals and and extra dose of protein for building strong muscles and repairing skin issues. An easy way to remember to drink the supplement would be to serve it when they are taking their medications, instead of water.
If your parent seem to be having more difficulty feeding themselves, you may want to seek the help of an occupational therapist that can recommend adaptive utensils that would allow your parent to maintain their independence for feeding. Eating is a pattern we develop very early on, so if your loved one can repattern themselves to put hand or fork to mouth, then they typically will eat more than when we are attempting to feed them, as some may find that mom or dad doesn’t open their mouths when the food is presented by someone else. If they are unable to hold a utensil due to arthritis, tremors, weakness, etc then throw away the fork all together and switch to “finger foods”. Opt for foods that they can pick up and eat with their hands, you may choose proteins such as chicken nuggets, fish sticks, or meatballs and vegetables like steamed carrots, green beans and broccoli. Or make everything into a sandwich, tuna fish, sloppy joes and egg salad sandwiches make great substitutes and can be less overwhelming and they even make kitchen devices that are specifically for that purpose. When you are making the weekly grocery run be sure to pick up plenty of healthy snacks that are easy to grab and go. Unless your parent has a specific health problem, the goal is to get them to consume more calories and the easier that is for them to do, the more successful you will become. Choose items like bananas, grapes, cheese sticks, or yogurt to encourage snacking throughout the day.
Lastly, talk with your doctor about the possible addition of an appetite stimulant. Some seniors to have success with prescription appetite stimulants, but it is important to consult with your doctor to make sure it is the right avenue to try. It will be important for you to have trialed multiple strategies prior to placing your parent on yet another medications, so keep track of what you’ve tried and how it worked. Keep experimenting with times and foods to determine your best outcomes and build on those things. Ask questions, observe behaviors and examine their mouths to ensure that you are getting all the information needed to determine why your parent has quit eating. In most cases, simply listening to your loved one and enlisting the help of a doctor, should lead you to to find a solution. Getting your loved one back into the routine of eating healthy quantities can help them live longer and enjoy life more. It’s worth it.
The information you need . . . Straight Up!

